Check out our latest blog article: From component to enterprise – modular robotics done right.
How Has Telehealth Evolved During the Pandemic, and What Comes Next?

The coronavirus pandemic has been exhausting healthcare systems all over the world since the beginning of 2020. New York City alone registered 51,178 coronavirus-related hospitalizations at the time of writing. Very few countries have enough healthcare workers to deal with such an increase. In Europe, for example, the number of doctors per 1000 population in Austria is quite high at 5.2, but in Turkey it's less than half that at only 1.9. Moreover, approximately one-third of those physicians are older than 55, which makes them susceptible to the coronavirus.
According to the International Council of Nurses, around 90,000 healthcare workers were infected with COVID-19 by the beginning of May, and more than 260 nurses died. To avoid unnecessary health risks for their employees, hospitals are now searching for a healthcare delivery method capable of minimizing in-person interactions and freeing hospital capacities.
Telehealth is emerging as a sustainable solution for the prevention and treatment of COVID-19, and management of all other health conditions not related to the coronavirus. Telehealth solutions help to triage patients while protecting medical staff, offer safe platforms for treating non-COVID diseases, and allow physicians to monitor patients with chronic conditions. Furthermore, it alleviates the strain on healthcare providers by allowing quarantined doctors to keep supporting their colleagues.
Telehealth Before 2020
Telehealth is defined as the use of digital communication technology to deliver healthcare services remotely. People tend to confuse telehealth with telemedicine. Telemedicine refers to patient-facing healthcare practices such as teleconsultation and remote patient monitoring. Telehealth is an umbrella term which encompasses telemedicine, but also expands to non-clinical services including administrative activities and training.
The first reference to telehealth dates back to 1955. Since then, the concept and its related technologies have come a long way.
The Nebraska Psychiatric Institute is reported to be the first medical facility to practice telehealth. Back in 1955, the Institute used a CCTV system and radio-transmitted records for patient treatment. Ultimately, the old system proved to be inefficient, and it wasn't until the digital age that interest in telehealth was revived.
Later in the 1960s and '70s, NASA, the Public Health Department, and other organizations invested heavily in telehealth. Those efforts resulted in the STARPPAHC project. It provided remote medical care to Native Americans on the Papago Reservation and astronauts in space.
Nowadays, with the advancements in technology, telehealth is thriving. It was gaining popularity even before COVID-19, as its adoption rate doubled between 2016 and 2019, representing the most substantial growth among digital healthcare tools.
Similar to the veterans, civilians are also enjoying remote healthcare services. The Telehealth Satisfaction Study conducted by JD Power revealed the overall satisfaction score among telehealth users was 851 on a 1000-point scale. This score was the highest JD Power observed on its healthcare, insurance, and financial service-related studies. 65% of the respondents mentioned they opted for telehealth after positive word of mouth from family and friends.
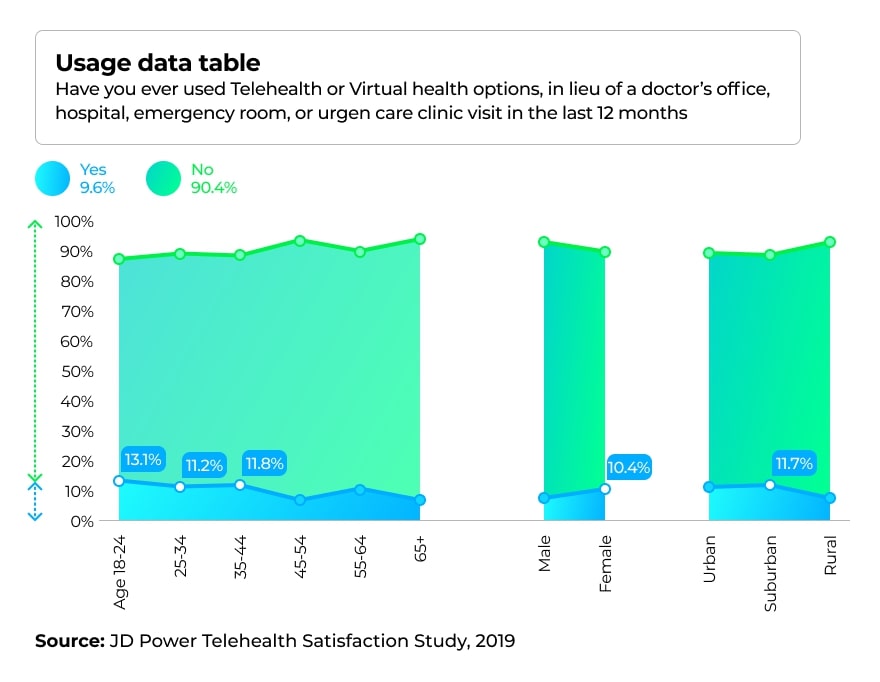
JD Power conducted another survey in 2019 to understand the pattern of telehealth usage. The graph below demonstrates that telehealth is mostly benefiting the age group (18-24), while the (45-54 and 65+) groups are less likely to try virtual doctor visits. Also, telehealth adoption is highest among suburban residents, not within rural area as one would expect.
Telehealth Use Cases
Initially, telehealth was perceived as a convenient healthcare delivery method for remote rural communities. However, as virtual health practices matured, its applications became more diverse. Now they include:
- Chronic disease management. With the help of medical Internet of Things, doctors can monitor patients with chronic conditions remotely. Patients equipped with specialized medical devices, such as smart blood pressure monitors, can measure their vitals and automatically transmit the results to their doctor.
- Physical therapy. Using videos, physicians can guide patients through physical exercises, correct their movements, and ensure completion of the prescribed physical therapy.
- Post-surgery monitoring. When there is no possibility of keeping patients hospitalized after surgery, telehealth tools may come in handy, and patients can be on a proper recovery path at home.
- Telepsychiatry. Consulting a psychiatrist remotely introduces a feeling of enhanced safety for some patients, making it easier for them to voice their concerns. Additionally, monitoring apps can detect disorders preemptively. For example, a California-based company, Mindstrong, found a way to recognize the first signs of depression and other mental health issues by monitoring how people use their phones.
Telehealth as a First Line of Defense Against COVID-19
Even though hospitals experimented with telehealth before the pandemic, now is the time when this approach really shines, and patients are actively seeking it. According to the latest SEMRush report, searches for "in-home doctor visit" spiked at 146.15% in February/March period, while "in-home medical care" searches increased by 55.79%.
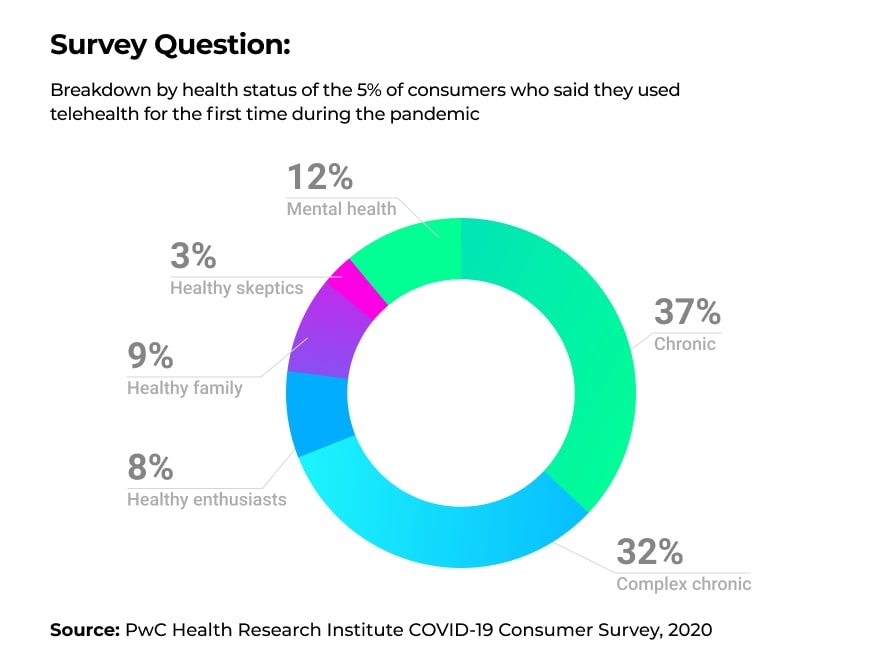
Despite the rise in search activity, the actual adoption of this technology is still moving slowly. Sykes, a customer experience IT vendor, surveyed 2,000 Americans regarding their telehealth usage in the COVID-19 era. Over 1,400 indicated they were not familiar with telehealth. 38% of the remaining respondents reported liking the idea of receiving care from the comfort of their home, while only 19% had actually tried teleconsultation. In parallel with Sykes, PwC's Health Research Institute surveyed around 2,500 respondents about their healthcare-related habits. Only 5% of the participants indicated they received telehealth consultation during the pandemic. Among those, 69% used telehealth for chronic disease management and 12% for mental health monitoring.
Official Support
The US government and prominent healthcare organizations are working towards facilitating telehealth adoption. In March, Congress approved around $500 million in emergency funding to cover the telehealth-related expenses of Medicare providers. Later that month, the White House signed the $2 trillion Coronavirus Aid, Relief, and Economic Security Act, which included a fund of $200 million for telehealth services.
Simultaneously, the Centers for Medicare and Medicaid Services lifted restrictions on reimbursements for telehealth services. Prior to this waiver, Medicare would only pay for telehealth services when the patient was residing in a designated remote area. With the new adjustment, healthcare providers will be paid for teleconsultation at the same rate as in-person visits regardless of the patient's location. Furthermore, the Department of Health and Human Services will relax privacy requirements on telehealth, allowing consultations to occur over Skype, FaceTime, Zoom, or any other commonly used platform.
As a last example, the American Medical Association updated its Telehealth Implementation Playbook Series. This guide contains best practices and tips on how to make the most out of telehealth technology.

Telehealth Use Cases to Battle the Coronavirus
The following applications demonstrate the importance of telehealth adoption:
- Benefiting from quarantined healthcare workers. Currently, many providers are self-isolating because of travel or exposure to the virus. The majority are either asymptomatic or experiencing mild symptoms, and are still able to perform their duties. These physicians can help their colleagues at the front line by offering advice and remotely monitoring COVID-19 patients.
- Assisting with mental health-related challenges. This is applicable for both the professionals battling the virus at the front line and the people struggling to remain quarantined in their homes. The mental health app Headspace is offering free premium services for healthcare providers throughout 2020. Moreover, meditation apps are now providing free subscriptions as relaxation lowers blood pressure and reduces the risk of cardiovascular diseases.
- Triaging patients. Tele-triage implies virtually screening patients with flu-like symptoms to understand who needs medical intervention and who can receive treatment at home. Dividing patients into risk and non-risk groups is a safe way to balance protecting hospital staff while still giving patients the treatment they need. Tele-triage helped Rush University Medical Center to avoid the fate of other hospitals where medical staff were subjected to a mass-quarantine after a patient tested positive for the coronavirus. Before arriving at Rush, the patient in question received a consultation with an infection specialist over an iPad and was diagnosed with COVID-19. Prior to the patient's arrival, the hospital cleared the ambulance bay from any staff or vehicles, and the patient was immediately transported to an isolated room where he was examined by an emergency physician wearing protective gear. The patient was treated and released without the infection spreading to staff members or other patients.
- Treating non-COVID patients.The chronically ill require constant monitoring, but they are also more susceptible to the virus. As a result, visiting healthcare facilities for consultation and medication prescription puts these patients under unnecessary risk. Using telehealth, they can schedule teleconsultation and have medication delivered to their door.
- Monitoring COVID-19 patients with mild symptoms while keeping them outside the hospital. Healthcare facilities do not have the capacity to hospitalize everyone who tested positive for the virus. Consequently, the patients who do not require intensive care may self-isolate at their homes while checking-in with their doctors via telehealth services. Armidale Hospital in Australia started a pilot program where doctors do not hospitalize COVID-19 patients with moderate symptoms, but instead, supply them with ICU-grade home monitors and send them back home. Healthcare practitioners continue tracking patients' vital signs remotely to detect any deterioration in condition as soon as it occurs.
Telehealth Benefits and Limitations
During the pandemic, telehealth has offered many perks to its users. Chief among the numerous telehealth benefits for providers is the fact that it allows clinical staff to be more productive. Instead of having a professional measure the vital signs, patients do this at home and transmit the results to a telehealth nurse. This means one nurse can manage a few hundred patients at a time. Another benefit is allowing seasoned physicians to help their less experienced colleagues in dispersed geographical locations.
Additionally, telehealth improves clinical outcomes as it helps doctors "see" patients more often. This healthcare delivery method allows more frequent checkups than would be possible with in-person meetings, which enables doctors to spot changes in patients as soon as they occur. Finally, with telehealth, patients can receive medical care from their homes, minimizing the risk of contracting the virus.
A considerable disadvantage of telehealth is that it cannot support COVID-19 testing, at least not in its current state.
Telehealth Forecast for the Post-Pandemic Era
Telehealth is not likely to fully replace in-person visits soon. Telehealth does not support physical examinations, and because healthcare professionals and their patients have often never met in person, they're likely to experience a delay building trust and empathy. However, the forecast for telehealth is understandably positive. The global telemedicine market is expected to skyrocket to over $175 billion by 2026 (up from $45 billion in 2019).
Whether telehealth will be widely adopted still depends considerably on the government. After the pandemic passes, authorities will be expected to relax the rules regarding where patients need to physically be to receive telehealth services, which healthcare professionals can offer telehealth consultations, and which treatments can be reimbursed. Also, restrictions are most likely to be placed on telehealth platforms to restore privacy.
Barriers to Telehealth Adoption
- Lack of infrastructure. Even though some telehealth practices are hardware-agnostic, the systems that incorporate high-resolution cameras and microphones provide a more accurate diagnosis and deliver better patient experience. Another related challenge is the need for a reliable internet connection. This is generally not a significant issue in urban areas, though the same cannot be said for the countryside. While large-scale programs for increasing wireless rural internet speeds are in the works, networks like global 5G and Starlink are still a ways off. Also, building design and acoustics within a doctor's office can be a factor in communication quality. For example, spacious concrete rooms often create an echo. This negative effect can be eliminated by placing soundboards.
- Threat of cyberattacks. Brno University Hospital is one of the largest COVID-19 testing centers in the Czech Republic. In March, the hospital was hit by a major cyberattack forcing all its computers to shut down. The incident prevented doctors from performing elective surgeries and restricted access to hospital lab data. For healthcare facilities implementing telehealth protocols, such cyberattacks are extremely dangerous. Hence, security teams need to be vigilant and well prepared to respond to intrusion attempts.
- Lack of affordability for some patients. Telehealth requires a modern smartphone and a reliable internet connection. Consequently, it might not be an option for low-income and non-tech-savvy users.
Adopting Telehealth in Your Clinic
After understanding what telehealth can do and realizing its benefits during the pandemic, patients and clinicians might be more forgiving of its current flaws. Consequently, healthcare organizations have to be prepared.
Incorporating telehealth practices into your clinic can be a daunting task. You need to notify patients, adjust your internal and patient-facing processes, learn about payer policies, and select your billing practices. Moreover, you need to find a reliable vendor to develop (or build on) the software and hardware of your telehealth solution. Below are some tips to get you started:
- Define your telehealth strategy. Determine where you fit in the market, which patient segments you are willing to serve, which technology you need to acquire, where to store your data, and how to address interoperability issues, etc.
- Prepare the workforce. Training employees is a considerable challenge. Some telehealth tech manufacturers supply introductory modules. But technology is not the only aspect to prepare for. Physicians need to practice their interaction with patients in the new format of virtual visits.
- Focus on both physicians' and patients' needs. Make sure that healthcare workers facing the patients are involved directly in the decision-making process, as they have a better understanding of what patients expect.
- Collaborate. Healthcare organizations cannot successfully implement telehealth in isolation. You need to partner with tech companies for acquisition and support of telehealth service technologies. In addition to this obvious collaboration, it can be beneficial to work with community service providers, retail pharmacies, and other organizations in the healthcare ecosystem.
If this seems overwhelming, keep in mind that telehealth is worth it in the end. Your patients and physicians will be enjoying the convenience it offers, and the availability of telehealth technologies can be a factor for customers searching for a healthcare provider. Additionally, many believe that this is not the last pandemic we are facing. If this is true, then healthcare facilities that fail to implement telehealth now will not be able to meet patients' expectations in the future.
More articles on the topic